Deep phenotyping of Post-infectious Myalgic Encephalomyelitis-Chronic Fatigue Syndrome
National Institutes of Health (NIH) conducted deep clinical and biological phenotyping using an extensive battery of tests to better understand Post-infectious/Myalgic Encephalomyelitis-Chronic Fatigue Syndrome
Dataset Overview
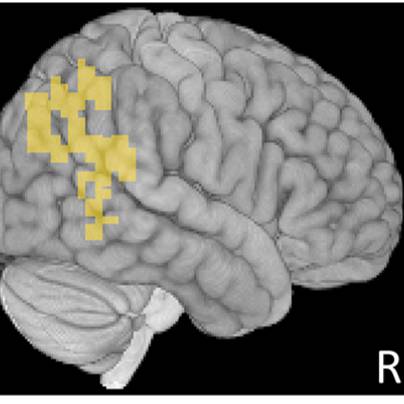
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a disabling disorder that may occur following an infection, yet the clinical phenotype is poorly defined, the pathophysiology is unknown, and no disease-modifying treatments are available. We used rigorous criteria to recruit a cohort of post-infectious ME/CFS (PI-ME/CFS) volunteers (n=17) with matched healthy controls (n=21) to conduct deep clinical and biological phenotyping using an extensive battery of tests. Among the many physical and cognitive complaints, one defining feature of PI-ME/CFS was an alteration of effort preference, rather than physical or central fatigue, due to dysfunction of integrative brain regions potentially associated with central catechol pathway dysregulation, with consequences on autonomic functioning and physical conditioning. Immune profiling suggested chronic antigenic stimulation with increase in naïve and decrease in switched memory B-cells. Alterations in gene expression profiles of peripheral blood mononuclear cells and metabolic pathways were consistent with cellular phenotypic studies and demonstrated differences according to sex. Together these clinical abnormalities and biomarker differences provide unique insight into the underlying pathophysiology of PI-ME/CFS, which may guide future intervention.
Files
1 - 0 of 0 files